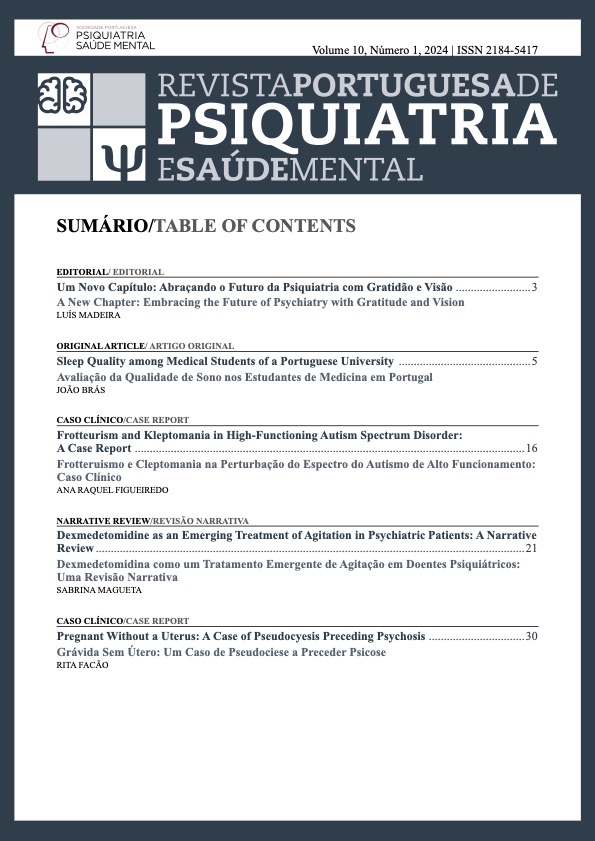
Dexmedetomidine as an Emerging Treatment of Agitation in Psychiatric Patients: A Narrative Review
DOI:
https://doi.org/10.51338/rppsm.506Keywords:
Dexmedetomidine/therapeutic use, Psychomotor Agitation/drug therapyAbstract
Acute agitation occurs in a variety of medical and psychiatric conditions and is the clinical presentation in a significant percentage of urgent psychiatric episodes, requiring prompt and effective intervention. Traditionally, agitation was managed in psychiatric wards using physical restraint. With the advent of tranquilizing neuroleptics, such as chlorpromazine, the pharmacological management of these conditions became possible. Acute agitation, although a potential result of most psychiatric disorders, is often associated with psychotic conditions, mood disorders and neurodegenerative disorders. The authors propose to explore dexmedetomidine as a therapeutic option in states of acute agitation in psychiatric patients in which traditional drugs are not effective. The authors based the work on a non-systematic review of the literature. Keywords used included: dexmedetomidine, acute agitation, rapid tranquilisation, restraint, sedation, psychiatric population and psychiatric disorders. Recently, a significant step forward in methods of treating acute agitation has been achieved through the use of dexmedetomidine in psychiatric patients. It is a selective α2‐receptor agonist being approved for short‐term sedation with the benefit of not having excessive sedation, thus allowing a concomitant psychotherapeutic approach. This proves to be a promising treatment option for those with acute agitation. The amount of studies available on its usefulness in psychiatric mental illness are still scarce. The interventional recommendations in the literature for agitation were developed based on research data, theoretical considerations and clinical experience, however, studies that provide definitive data are needed. It is imperative that the investigation of episodes of acute agitation and their restraint evolve, in order to protect these patients from the consequences of this behaviour and its treatment. Exploring the potential of dexmedetomidine as a tool in the mental health professional’s kit is well deserved as there are few alternatives that reassure the highly agitated patient without excessive sedation.Downloads
References
Rojas-Velasquez, Danilo Alejandro. The Evolution of Restraint in American Psychiatry. [Yale Medicine Thesis Digital Library]. Yale: YM; 2017. [accessed Jun 2022] Available at: https://elischolar.library.yale. edu/ymtdl/2167
Almeida M, Cicolello K, Hanso A, DeCavalcante G, DeOliveira GS. Treatment of Acute Agitation Associated With Excited Catatonia Using Dexmedetomidine: Case Series and Literature Review. Prim Care Companion CNS Disord. 2021;23:20cr02899. doi: 10.4088/PCC.20cr02899.
San L, Marksteiner J, Zwanzger P, Figuero MA, Romero FT, Kyropoulos G, et al. State of Acute Agitation at Psychiatric Emergencies in Europe: The STAGE Study. Clin Pract Epidemiol Ment Health. 2016;12:75-86. doi: 10.2174/1745017901612010075.
Pompili M, Ducci G, Galluzzo A, Rosso G, Palumbo C, De Berardis D. The Management of Psychomotor Agitation Associated with Schizophrenia or Bipolar Disorder: A Brief Review. Int J Environ Res Public Health. 2021;18:4368. doi: 10.3390/ijerph18084368.
Garriga M, Pacchiarotti I, Kasper S, Zeller SL, Allen MH, Vázquez G, et al. Assessment and management of agitation in psychiatry: Expert consensus. World J Biol Psychiatry. 2016;17:86-128. doi: 10.3109/15622975.2015.1132007.
Novitayani S, Aiyub M. Restraint in Psychiatric Patients: A Literature Review. In: Proceedings of the Aceh International Nursing Conference - Volume 1. AINC; 2018. doi: 10.5220/0008396900002442
Harwood RH. How to deal with violent and aggressive patients in acute medical settings. J R Coll Physicians Edinb. 2017;47:94-101. doi: 10.4997/ JRCPE.2017.218.
Negroni A. On the concept of restraint in psychiatry. Eur J Psychiatry. 2017;31:99-104. doi: 10.1016/j. ejpsy.2017.05.001.
Wynn R. Medicate, restrain or seclude? Strategies for dealing with violent and threatening behaviour in a Norwegian university psychiatric hospital. Scand J Caring Sci. 2002;16:287-91. doi: 10.1046/j.1471-6712.2002.00082.x.
Ramachandraiah CT, Subramaniam N, Tancer M. The story of antipsychotics: Past and present. Indian J Psychiatry. 2009;51:324-6. doi: 10.4103/0019-5545.58304.
Hsiao JK. Sublingual Dexmedetomidine as a Potential New Treatment for Agitation. JAMA. 2022;327:723– 25. doi:10.1001/jama.2021.21313
Richmond JS, Berlin JS, Fishkind AB, Holloman GH Jr, Zeller SL, Wilson MP, et al. Verbal De-escalation of the Agitated Patient: Consensus Statement of the American Association for Emergency Psychiatry Project BETA De-escalation Workgroup. West J Emerg Med. 2012;13:17-25. doi: 10.5811/westjem.2011.9.6864.
Abrahamsen C. 2002 guide to new technologypatient restraint: JCAHO and HCFA isuue new restraint guideline. Nurs Manag.2001;32:69-70
Mohr WK, Petti TA, Mohr BD. Adverse effects associated with physical restraint. Can J Psychiatry. 2003;48:330-7. doi: 10.1177/070674370304800509.
Mohr WK, Mahon MM, Noone MJ. A restraint on restraints: the need to reconsider restrictive interventions. Arch Psychiatr Nurs. 1998;12:95–106. 7.
Gallop R, McKay E, Guha M, Khan P. The experience of hospitalization and restraint of women who have a history of childhood sexual abuse. Health Care Women Int. 1999;20:401–16.
Asher L, Fekadu A, Teferra S, De Silva M, Pathare S, Hanlon C. “I cry every day and night, I have my son tied in chains”: physical restraint of people with schizophrenia in community settings in Ethiopia. Global Health. 2017;13:47. doi: 10.1186/s12992-017-0273-1.
Mohr WK, Pumariega AJ. Post restraint sequelae five years out: concerns and policy implications. Paper presented at the Annual American Psychiatric Association Meeting; May 9, 2001; New Orleans.
Bosch OG, Dornbierer DA, Bavato F, Quednow BB, LandoltHP,SeifritzE.DexmedetomidineinPsychiatry: Repurposing of its Fast-Acting Anxiolytic, Analgesic and Sleep Modulating Properties. Pharmacopsychiatry. 2023;56:44-50. doi: 10.1055/a-1970-3453.
Mo Y, Zimmermann AE. Role of dexmedetomidine for the prevention and treatment of delirium in intensive care unit patients. Ann Pharmacother. 2013;47:869–76
Chail A, Dubey A, Singh YM, Jahan N. Adjunctive dexmedetomidine for treatment of delirium tremens: Case report and brief review. Ind Psychiatry J. 2019;28:321-4. doi: 10.4103/ipj.ipj_118_20.
Faden J, Musselman M, Citrome L. Sublingual dexmedetomidine: repurposing an anesthetic as an anti-agitation agent. Expert Rev Neurother. 2023;23:97-106. doi: 10.1080/14737175.2023.2174430.
Mahmoud M, Mason KP. Dexmedetomidine: review, update, and future considerations of paediatric perioperative and periprocedural applications and limitations. Br J Anaesth. 2015;115:171-82. doi: 10.1093/bja/aev226.
Ramaswamy SM, Weerink MAS, Struys MM, Nagaraj SB. Dexmedetomidine-induced deep sedation mimics non-rapid eye movement stage 3 sleep: large-scale validation using machine learning. Sleep. 2021;44:zsaa167. doi: 10.1093/sleep/zsaa167.
Shapiro FE. Manual of Office‐Based Anesthesia Procedures. London: Lippincott Williams & Wilkins; 2007.
Zhao Y, He J, Yu N, Jia C, Wang S. Mechanisms of Dexmedetomidine in Neuropathic Pain. Front Neurosci. 2020;14:330. doi: 10.3389/fnins.2020.00330.
Virtanen R, Savola JM, Saano V, Nyman L. Characterization of the selectivity, specificity and potency of medetomidine as an alpha 2-adrenoceptor agonist. Eur J Pharmacol. 1988;150:9–14.
Ebert TJ, Hall JE, Barney JA. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000;93:382–94
Anttila M, Penttilä J, Helminen A, Vuorilehto L, Scheinin H. Bioavailability of dexmedetomidine after extravascular doses in healthy subjects. Br J Clin Pharmacol. 2003;56:691–3.
Yoo H, Iirola T, Vilo S, Manner T, Aantaa R, Lahtinen M, et al. Mechanism-based population pharmacokinetic and pharmacodynamic modeling of intravenous and intranasal dexmedetomidine in healthy subjects. Eur J Clin Pharmacol. 2015;71:1197–207.
US Food and Drug Administration. Precedex label. 1999. Available from: http://www.accessdata.fda.gov/ drugsatfda_docs/label/1999/21038lbl.pdf;
European Medicines Agency. European Public Assessment Report. 2016. [accessed Jan 2023] Available from: http://www.ema.europa.eu/docs/en_GB/ document_library/EPAR__Product_Information/human/002268/WC500115631.pdf
Cunningham FE, Baughman VL, Tonkovich L. Pharmacokinetics of dexmedetomidine (DEX) in patients with hepatic failure (HF). Clin Pharmacol Ther. 1999;65:128.
Karol MD, Maze M. Pharmacokinetics and interaction pharmacodynamics of dexmedetomidine in humans. Best Pract Res Clin Anaesthesiol. 2000;14:261–9.
Chang ET, Certal V, Song SA, Zaghi S, Carrasco-Llatas M, Torre C, et al. Dexmedetomidine versus propofol during drug-induced sleep endoscopy and sedation: a systematic review. Sleep Breath. 2017;21:727-35. doi: 10.1007/s11325-017-1465-x.
Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007;298:2644-53. doi: 10.1001/jama.298.22.2644.
Smithburger PL, Smith RB, Kane-Gill SL, Empey PE. Patient predictors of dexmedetomidine effectiveness for sedation in intensive care units. Am J Crit Care. 2014;23:160–5.
Sallinen J, Hoglund I, Engstrom M, Lehtimäki J, Virtanen R, Sirviö J, et al. Pharmacological characterization and CNS effects of a novel highly selective a2C-adrenoceptor antagonist JP-1302. Br J Pharmacol. 2007;150:391–402.
Neumeister A, Drevets WC, Belfer I, Luckenbaugh DA, Henry S, Bonne O, et al. Effects of a alpha(2C)-adrenoreceptor gene polymorphism on neural responses to facial expressions in depression. Neuropsychopharmacology. 2006;31:1750–6. doi: 10.1038/sj.npp.1301010.
Drug Guideline: Dexmedetomidine. Version 3. [accessed May 2023]. Available from: https://www.bhs. org.au/bhsapps/govdoc/gdhtml/gddrg0056--25290-dexmedetomidine%20final%20for%20spice%20 iv%20trial%20040722.pdf
Drug Interactions between dexmedetomidine and Valproate Sodium. [accessed Oct 2023]. Available from: https:// www.drugs.com/drug-interactions/dexmedetomidine-with-valproate-sodium-835-0-2286-17497.html
Reel B, Maani CV. Dexmedetomidine. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2023. [accessed May 2023]. Available from: https://www.ncbi.nlm.nih.gov/books/ NBK513303.
Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263–306.
Dexmedetomidine Pregnancy and Breastfeeding Warnings. [accessed Oct 2023]. Available from: https:// www.drugs.com/pregnancy/dexmedetomidine.html.
Lactation sources: Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Library of Medicine (US); 2006. [accessed Oct 2023]. Available from: https://www.ncbi.nlm.nih.gov/books/ NBK501922/1.
Nakanishi R, Yoshimura M, Suno M, Yamamoto K, Ito H, Uchimine Y, et al. Detection of dexmedetomidine in human breast milk using liquid chromatography-tandem mass spectrometry: Application to a study of drug safety in breastfeeding after Cesarean section. J Chromatogr B Analyt Technol Biomed Life Sci. 2017;1040:208-13. doi: 10.1016/j. jchromb.2016.11.015.
Yoshimura M, Kunisawa T, Suno M, Sugawara A, Kurosawa A, Nakanishi R, et al. Intravenous dexmedetomidine for cesarean delivery and its concentration in colostrum. Int J Obstet Anesth. 2017;32:28-32. doi: 10.1016/j.ijoa.2017.05.002.
Dyck JB, Maze M, Haack C, Vuorilehto L, Shafer SL. The pharmacokinetics and hemodynamic effects of intravenous and intramuscular dexmedetomidine hydrochloride in adult human volunteers. Anesthesiology. 1993;78:813–20.
European Medicines Agency. European Public Assessment Report. 2016. [accessed Oct 2023]. Available from: http://www.ema.europa.eu/docs/en_GB/ document_library/EPAR_-_Product_Information/ human/002268/WC500115631.pdf.
Aksay SS, Bumb JM, Remennik D, Thiel M, Kranaster L, Sartorius A, Janke C. Dexmedetomidine for the management of postictal agitation after electroconvulsive therapy with S-ketamine anesthesia. Neuropsychiatr Dis Treat. 2017;13:1389-1394 doi: 10.2147/NDT.S134751
Brydges D, Tibrewal P, Waite S, Dhillon R. Use of dexmedetomidine in treatment-refractory post-electroconvulsive therapy agitation.Aust N Z J Psychiatry. 2016;50:386-7. doi:10.1177/0004867415610638
Narango P, Ianovich F, Sarai SK, Lippmann S. Benefits of dexmedetomidine in management of post‐ECT agitation. J ECT. 2017;33:150–1.
Nelson S, Muzyk AJ, Bucklin MH, Brudney S, Gagliardi JP. Defining the role of dexmedetomidine in the prevention of delirium in the intensive care unit. Biomed Res Int. 2015;2015:635737. doi: 10.1155/2015/635737.
Muzyk AJ, Fowler JA, Norwood DK, Chilipko A. Role of α2‐agonists in the treatment of acute alcohol withdrawal. Ann Pharmacother. 2011;45:649–57. doi: 10.1345/aph.1P575.
Muzyk AJ, Revollo JY, Rivelli SK. The use of dexmedetomidine in alcohol withdrawal. J Neuropsychiatry Clin Neurosci. 2012;24:E45–6. doi: 10.1176/appi. neuropsych.11080194.
Louis C, Godet T, Chanques G, Bourguignon N, Morand D, Pereira B, et al. Effects of dexmedetomidine on delirium duration of non-intubated ICU patients (4D trial): study protocol for a randomized trial. Trials. 2018;19:307. doi: 10.1186/s13063-018-2656-x.
Reade MC, O’Sullivan K, Bates S, Goldsmith D, Ainslie WR, Bellomo R. Dexmedetomidine vs. haloperidol in delirious, agitated, intubated patients: a randomised open-label trial. Crit Care. 2009;13:R75.
Maldonado JR, Wysong A, van der Starre PJ, Block T, Miller C, Reitz BA. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009;50:206–17.
Rovasalo A, Tohmo H, Aantaa R, et al. Dexmedetomidine as an adjuvant in the treatment of alcohol withdrawal delirium: a case report. Gen Hosp Psychiatry. 2006;28(4):362–363
Citrome L, Preskorn SH, Lauriello J, Krystal JH, Kakar R, Finman J, et al. Sublingual Dexmedetomidine for the Treatment of Acute Agitation in Adults With Schizophrenia or Schizoaffective Disorder: A Randomized Placebo-Controlled Trial. J Clin Psychiatry. 2022;83:22m14447. doi: 10.4088/JCP.22m14447.
BioXcel Therapeutics, author. IGALMITM (dexmedetomidine) sublingual film, for sublingual or buccal use [Internet] Bethesda: Silver Spring: Food and Drug Administration; 2022.
Yocca F, DeVivo M, Seth S, Sharma S. Dexmedetomidine—highly favorable pharmacokinetic and pharmacological features for a CNS therapeutic drug. Poster presented: at the 58th Annual meeting of the American College of Neuropsychopharmacology; December 8-11, 2019; Orlando, FL.
Zareifopoulos N, Panayiotakopoulos G. Treatment options for acute agitation in psychiatric patients: theoretical and empirical evidence. Cureus. 2019;11:e6152. doi: 10.7759/cureus.6152.
Smith CM, Santalucia M, Bunn H, Muzyk A. Sublingual Dexmedetomidine for the Treatment of Agitation in Patients with Schizophrenia and Bipolar Disorder. Clin Psychopharmacol Neurosci 2023;21:215-221. doi:10.9758/cpn.2023.21.2.215
Henry PH, Dantz B. Sublingual Dexmedetomidine vs Placebo and Acute Agitation Associated With Bipolar Disorder. JAMA. 2022;328:213-4. doi: 10.1001/ jama.2022.8352.
Ward K, Citrome L. The treatment of acute agitation associated with schizophrenia or bipolar disorder: investigational drugs in early stages of their clinical development, and their clinical context and potential place in therapy. Expert Opin Investig Drugs. 2020;29:245-57. doi: 10.1080/13543784.2020.1727884.
Qu JZ, Mueller A, McKay TB, Westover MB, Shelton KT, Shaefi S, et al. Nighttime dexmedetomidine for delirium prevention in non-mechanically ventilated patients after cardiac surgery (MINDDS): A single-centre, parallel-arm, randomised, placebo-controlled superiority trial. EClinicalMedicine. 2022;56:101796. doi: 10.1016/j.eclinm.2022.101796.
VanderWeide LA, Foster CJ, MacLaren R, Kiser TH, Fish DN, Mueller SW. Evaluation of Early Dexmedetomidine Addition to the Standard of Care for Severe Alcohol Withdrawal in the ICU: A Retrospective Controlled Cohort Study. J Intensive Care Med. 2016;31:198-204. doi: 10.1177/0885066614554908.
Walker A, Delle Donne A, Douglas E, Spicer K, Pluim T. Novel use of dexmedetomidine for the treatment of anticholinergic toxidrome. J Med Toxicol. 2014;10:406-10. doi: 10.1007/s13181-014-0408-1.