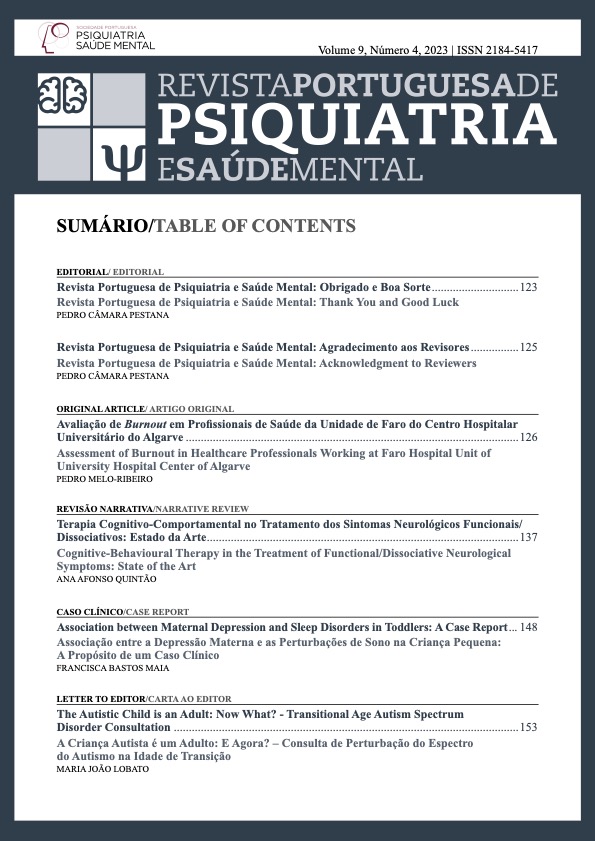
Cognitive‐Behavioural Therapy in the Treatment of Functional/Dissociative Neurological Symptoms: State of the Art
DOI:
https://doi.org/10.51338/rppsm.508Keywords:
Cognitive Behavioral Therapy, Conversion Disorder, Dissociative DisordersAbstract
Introduction: The functional/dissociative neurological symptoms (F/DNS) generate disability and decrease productivity and quality of life. The therapeutic approach is still unclear; cognitive-behavioural therapy (CBT) seems to yield positive results. This review aims to summarize evidence on the effectiveness of CBT on the treatment of F/DNS.Methods: Non-systematic review of the literature; search on the PubMed/Medline database, using PRISMA guidelines for scoping reviews, with terms related to F/DNS and CBT.
Results: Several studies describe advantages of CBT in the treatment of functional tremor; postural-perceptive persistent dizziness; non-epileptic psychogenic seizures; several functional movement disorders; and F/DNS in general, with improvement in primary (reduction in physical symptoms) and secondary outcomes (functioning level, quality of life, mental state, anxiety/depression, service use). Some studies analysed psychological interventions globally, and not CBT specifically. One review about neuromodulation for the treatment of F/DNS states that its efficacy is unproven; they speculate that the combination with CBT might be promising.
Discussion: Recent studies state that, globally, there is little high-quality evidence; they consider that some studies have a high risk of bias and lack an appropriate analysis of the quality of evidence. Some contradictions between studies have been found, for example regarding improvement of functioning level and reduction of the number of convulsions. However, most studies report some evidence on the efficacy of CBT in the treatment of different F/DNS, regarding primary and secondary outcomes, some in combination with physiotherapy and other psychotherapeutic modalities, reinforcing the importance of a multidisciplinary approach.
Conclusion: The studies conducted to date exhibit significant methodological issues, including a low number of included patients and patient heterogeneity, making it challenging to compare studies and obtain high-quality methodological research. Although there is no consensus on the best therapeutic approach, and despite the low methodological quality existing thus far, CBT is the approach that has shown the best results (in primary and secondary outcomes) in the treatment of F/DNS. Additional studies with methodological rigor are needed to validate the positive results obtained thus far.
Downloads
References
Edwards MJ, Bhatia KP. Functional (psychogenic) movement disorders: merging mind and brain. Lancet Neurol. 2012;11:250-60. doi:10.1016/ S1474-4422(11)70310-6
Stone J, Wojcik W, Durrance D, Carson A, Lewis S, MacKenzie L, et al. What should we say to patients with symptoms unexplained by disease? The “number needed to offend.” BMJ. 2002;325:1449-50. doi: 10.1136/bmj.325.7378.1449.
The ICD‐11 Classification of Mental and Behavioural Disorders – Diagnostic criteria for research. 11th edition. Geneva: World Health Organization; 2018.
Diagnostic and Statistical Manual of Mental Disorders, DSM-5-TR. 5th edition-Text Revision. Chicago: American Psychiatric Publishing; 2013.
Hallett M, Aybek S, Dworetzky BA, McWhirter L, Staab J, Stone J. Functional Neurological Disorder: New Phenotypes, Common Mechanisms. Lancet Neurol. 2022;21:537-50. doi:10.1016/S1474-4422(21)00422-1
Duncan R, Razvi S, Mulhern S. Newly presenting psychogenic nonepileptic seizures: incidence, population characteristics, and early outcome from a prospective audit of a first seizure clinic. Epilepsy Behav. 2011;20:308-11. doi:10.1016/j.yebeh.2010.10.022
Goldstein LH, Deale AC, Mitchell-O’Malley SJ, Toone BK, Mellers JD. An evaluation of cognitive behavioral therapy as a treatment for dissociative seizures: a pilot study. Cogn Behav Neurol. 2004;17:41-9. doi:10.1097/00146965-200403000-00005
Erro R, Brigo F, Trinka E, Turri G, Edwards MJ, Tinazzi M. Psychogenic nonepileptic seizures and movement disorders. Neurol Clin Pract. 2016;6:138-49. doi:10.1212/CPJ.0000000000000235.
Geddes JR, Andreasen NC, Goodwin GM. New Oxford Textbook of Psychiatry.3rd ed. Oxford:Oxford University Press; 2020.
Stone J, Sharpe M, Binzer M. Motor conversion symptoms and pseudoseizures: a comparison of clinical characteristics. Psychosomatics. 2004;45:492-9. doi:10.1176/appi.psy.45.6.492
Edwards MJ, Yogarajah M, Stone J. Why functional neurological disorder is not feigning or malingering. Nat Rev Neurol. 2023;19:246-56. doi:10.1038/ s41582-022-00765-z
Morgante F, Edwards MJ, Espay AJ. Psychogenic movement disorders. Continuum.2013;191383-96. doi:10.1212/01.CON.0000436160.41071.79
LaFrance Jr. WC, Baker GA, Duncan R, Goldstein LH, Reuber M. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: A staged approach. Epilepsia. 2013;54:2005-18. doi:10.1111/epi.12356
Avbersek A, Sisodiya S. Does the primary literature provide support for clinical signs used to distinguish psychogenic nonepileptic seizures from epileptic seizures? J Neurol Neurosurg Psychiatry. 2010;81:719-25. doi:10.1136/jnnp.2009.197996
Gonsalvez I, Spagnolo P, Dworetzky B, Baslet G. Neurostimulation for the treatment of functional neurological disorder: A systematic review. Epilepsy Behav Rep. 2021;16:100501. doi:10.1016/j.ebr.2021.100501
Martlew J, Pulman J, Marson AG. Psychological and behavioural treatments for adults with non-epileptic attack disorder. Cochrane Database Syst Rev. 2014:CD006370. doi:10.1002/14651858.CD006370.pub2
Beck AT, Haigh EA. Advances in cognitive theory and therapy: the generic cognitive model. Annu Rev Clin Psychol. 2014;10:1-24. doi:10.1146/ annurev-clinpsy-032813-153734
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
Bartl M, Kewitsch R, Hallett M, Tegenthoff M, Paulus W. Diagnosis and therapy of functional tremor a systematic review illustrated by a case report. Neurol Res Pract. 2020;2:35. doi:10.1186/s42466-020-00073-1
Espay AJ, Ries S, Maloney T, Vannest J, Neefus E, Dwivedi AK, et al. Clinical and neural responses to cognitive behavioral therapy for functional tremor. Neurology. 2019;93:e1787-98. doi:10.1212/ WNL.0000000000008442
Trinidade A, Goebel JA. Persistent postural-perceptual dizziness-a systematic review of the literature for the balance specialist. Otol Neurotol. 2018;39:1291-303. doi:10.1097/MAO.0000000000002010
Holmberg J, Karlberg M, Harlacher U, Rivano-Fischer M, Magnusson M. Treatment of phobic postural vertigo. A controlled study of cognitive-behavioral therapy and self-controlled desensitization. J Neurol. 2006;253:500-6. doi:10.1007/s00415-005-0050-6
Schmid DA, Allum JHJ, Sleptsova M, Gross S, Gaab J, Welge-Lüssen A, et al. Effects of a program of cognitive-behavioural group therapy, vestibular rehabilitation, and psychoeducational explanations on patients with dizziness and no quantified balance deficit, compared to patients with dizziness and a quantified balance deficit. J Psychosom Res. 2018;105:21‐30. doi:10.1016/j.jpsychores.2017.11.020
Yu YC, Xue H, Zhang YX, Zhou J. Cognitive behavior therapy as augmentation for sertraline in treating patients with persistent postural-perceptual dizziness. Biomed Res Int. 2018;2018:8518631. doi:10.1155/2018/8518631
Gutkin M, McLean L, Brown R, Kanaan RA. Systematic review of psychotherapy for adults with functional neurological disorder. J Neurol Neurosurg Psychiatry. Published online November 5, 2020:jnnp-2019-321926. doi:10.1136/jnnp-2019-321926
Goldstein LH, Chalder T, Chigwedere C, Khondoker MR, Moriarty J, Toone BK, et al. Cognitive-behavioral therapy for psychogenic nonepileptic seizures: a pilot RCT. Neurology. 2010;74:1986-94. doi:10.1212/ WNL.0b013e3181e39658
Goldstein LH, Robinson EJ, Mellers JDC, Stone J, Carson A, Reuber M, et al. Cognitive behavioural therapy for adults with dissociative seizures (CODES): a pragmatic, multicentre, randomised controlled trial. Lancet Psychiatry. 2020;7:491-505. doi:10.1016/ S2215-0366(20)30128-0
LaFrance WC, Baird GL, Barry JJ, Blum AS, Webb AF, Keitner GI, et al. Multicenter pilot treatment trial for psychogenic nonepileptic seizures: a randomized clinical trial. JAMA Psychiatry. 2014;71:997-1005. doi:10.1001/jamapsychiatry.2014.817
Sharpe M, Walker J, Williams C, Stone J, Cavanagh J, Murray G, et al. Guided self-help for functional (psychogenic) symptoms: a randomized controlled efficacy trial. Neurology. 2011;77:564‐72. doi:10.1212/ WNL.0b013e318228c0c7
Dallocchio C, Tinazzi M, Bombieri F, Arnó N, Erro R. Cognitive Behavioural Therapy and Adjunctive Physical Activity for Functional Movement Disorders (Conversion Disorder): A Pilot, Single-Blinded, Randomized Study. Psychother Psychosom. 2016;85:381-83. doi:10.1159/000446660
Carlson P, Nicholson Perry K. Psychological interventions for psychogenic non-epileptic seizures: A meta-analysis. Seizure. 2017;45:142-50. doi:10.1016/j. seizure.2016.12.007
Berezowski L, Ludwig L, Martin A, Löwe B, Shedden-Mora MC. Early psychological interventions for somatic symptom disorder and functional somatic syndromes: a systematic review and meta-analysis. Psychosom Med. 2022;84:325-38. doi:10.1097/ PSY.0000000000001011
Ludot M, Merlo M, Ibrahim N, Piot MA, Lefèvre H, Carles ME, et al. “Somatic symptom disorders” in adolescence. A systematic review of the recent literature. Encephale. 2021;47:596-604. doi:10.1016/j. encep.2021.04.007
Vugts MAP, Joosen MCW, van der Geer JE, Zedlitz AM, Vrijhoef HJ. The effectiveness of various computer-based interventions for patients with chronic pain or functional somatic syndromes: A systematic review and meta-analysis. PLoS One. 2018;13:e0196467. doi:10.1371/journal.pone.0196467
Rosendal M, Blankenstein AH, Morriss R, Fink P, Sharpe M, Burton C. Enhanced care by generalists for functional somatic symptoms and disorders in primary care. Cochrane Database Syst Rev. 2013:CD008142. doi:10.1002/14651858.CD008142.pub2
Ganslev CA, Storebø OJ, Callesen HE, Ruddy R, Søgaard U. Psychosocial interventions for conversion and dissociative disorders in adults. Cochrane Database Syst Rev. 2020;7:CD005331. doi:10.1002/14651858. CD005331.pub3
Aamir S, Hamayon S. Behavior therapy in dissociative convulsion disorder. J Depress Anxiety. 2012;01. doi:10.4172/2167-1044.1000103
Khattak T, Farooq S, Jan B. Behavior therapy in dissociative convulsions disorder. J Coll Physicians Surg Pak. 2006;16:359-63.
Jordbru AA, Smedstad LM, Klungsøyr O, Martinsen EW. Psychogenic gait disorder: a randomized controlled trial of physical rehabilitation with one-year follow-up. J Rehabil Med. 2014;46:181-7. doi:10.2340/16501977-1246
Nielsen G, Buszewicz M, Stevenson F, Hunter R, Holt K, Dudziec M, et al. Randomised feasibility study of physiotherapy for patients with functional motor symptoms. J Neurol Neurosurg Psychiatry. 2017;88:484-90. doi:10.1136/jnnp-2016-314408
Tolchin B, Baslet G, Suzuki J, Martino S, Blumenfeld H, Hirsch LJ, et al. Randomized controlled trial of motivational interviewing for psychogenic nonepileptic seizures. Epilepsia. 2019;60:986-95. doi:10.1111/ epi.14728